Significant advances in cancer treatment have meant that more patients are cured and many live longer than in the past. But it is still the case that we shall die.
a white paper on relieving the treatment and care is full of good words, but the proposals should be based on the evidence and the advice in the NOU 2017:16 "life and death". This know patients in Norway on the body every day.
Dagbladet Magazine set the spotlight on this now for the weekend with the story of three terminally ill cancer patients. We who work with pain relief – palliasjon – experience this up close. The destinies is strong. It's about life – what kind of life one may be able to live – before death arises.
A patient with bukspyttkjertelkreft tell us about their experiences: "I want to live, even though I know that I shall die soon. Can you give me a treatment that I can live as normally and well as possible? I will follow up my projects that are important to me. I will still be physically active, go for walks with my skivenner and grandchildren. I will not be at the hospital, but have you guys there when it is needed. I need to feel confident that you can what you are doing, so it does not become such as I experienced when my father died. He had excruciating pain over long periods of time and the doctor did not talk with us about the father's situation. I think she was afraid to talk with us, because she didn't know how she could help us. Too much was left to us in the family. That is what I am afraid will happen with me and my family"
The most important desired DebatePatients fear pain and other distressing symptoms, to be alone, to be dependent on help from others, loneliness, and family and children's life after death. This is a difficult time to master. Good mastery is a prerequisite for being able to live as well as possible for the patient, and that that the family can remember a difficult time in a best possible way.
Patients want to be home as much and for as long as possible when one is seriously ill, whether he/she has a short or long life expectancy. But this must be planned early and be based on your wishes. It often requires the expertise of specialists in relief (palliasjon) has to help the doctor, hjemmesykepleie and other hjelpepersonell where the patient is and will be.
A forward-looking palliativt offers must be further developed based on our public health care system with a better interaction between the specialist and municipal health service). The goal must be the right skills, in the right place, at the right time.
Field palliasjon is one of the fastest growing specialty areas in many countries in Europe, the USA, Canada and Japan. Several studies have shown that good palliasjon planned and carried out by competent personnel, provides a better quality of life for the patient and the family, more hjemmetid – and some studies have also shown prolonged life.
This is the Ingers avskjedsbrev DebateWhy choose when the government opposite strategy in its white paper by marginalising the need for knowledge? The message is not future proof and will not contribute to a good enough offer to Norwegian patients.
We would like to point to some examples of clear diskrepanser between the NOU and the white paper:
the Committee suggested a separate medical specialty as a continuation of the current trial with his area of expertise. This wants the government to investigate because they believe that: "A own specialty will not be able to resolve your clients' need for expertise in this area .... The need for such skills must therefore first and foremost meet to further develop the competence in palliasjon within the already existing medical specialties .....".
This is a alminneliggjøring of a discipline that also requires specialised expertise. If you do not have an active academic environment with academic development and research, so it is hard to see how this competence is distributed, should come from. The field has been uncertain and it will decrease the recruitment to a field of study which will be without specialists. The competency palliasjon is not even mentioned in the white paper. The doctors will bet on a field that is so controversial?
Good organisation shall ensure good exercise. Much of NOU-a reviews how the organisation based on today's great structures, can be developed. In parts of the country is this well organized in the day, while others have major deficiencies that contribute to unwanted variation.
A concrete action in the message could be to ensure that all health organisations created palliative organization in line with what is recommended in NOU-a. For the University hospital in Northern Norway, the current signals from the government is likely to mean that one establishes a provision for children, without having a well-functioning regional palliativt center for the largest group of patients, adults.
In practice, when the northern region are still left without a regional offer in the palliasjon for the adults while the government supports the barnehospice in Kristiansand and other random hospicetiltak.
She has everything, "the dictator" missing Commentregional kompetansetjenestene for relieving treatment has largely functioned as a competence - and /or forskningsbasene in palliasjon in large parts of the country. It was put forward concrete proposals in NOU-a about the strengthening of these, but kompetansetjenestene is barely mentioned. Many of the suggestions for improvement that are mentioned in the white paper, is it kompetansetjenestene which largely coordinates and performs today.
Field palliasjon is a young discipline. In the white paper shows that there is a lack good research that can form the basis for good fagutøvelse and that can reveal unwanted variations in quality. It was put forward several concrete proposals for the strengthening of research in relieving treatment, without this being taken to follow.
most of The points that were proposed by the committee, it is not associated with a specific proposal. The measures and the facility in The white paper need to be improved, often with suggestions from the NOU-a. Then we can together develop the best offer to our population.
Message to up to treatment in the fall. From now until the, have the politicians the opportunity to follow up with concrete measures that can contribute to better soothing treatment for the seriously ill, the dying and their families.
The white paper is not clear or ambitious enough for a time to perpetuate the lack of provision we have today, and it is incomprehensible in light of the documented gains. Patients and families will not get the offer they badly need from the Norwegian health care system and more people will therefore die with ailments that could have been alleviated. the
Want to discuss?
Visit Dagbladet debate!
 Exploring Cardano: Inner Workings and Advantages of this Cryptocurrency
Exploring Cardano: Inner Workings and Advantages of this Cryptocurrency Seville.- Economy.- Innova.- STSA inaugurates its new painting and sealing hangar in San Pablo, for 18 million
Seville.- Economy.- Innova.- STSA inaugurates its new painting and sealing hangar in San Pablo, for 18 million Innova.- More than 300 volunteers join the Andalucía Compromiso Digital network in one month to facilitate access to ICT
Innova.- More than 300 volunteers join the Andalucía Compromiso Digital network in one month to facilitate access to ICT Innova.-AMP.- Ayesa acquires 51% of Sadiel, which will create new technological engineering products and expand markets
Innova.-AMP.- Ayesa acquires 51% of Sadiel, which will create new technological engineering products and expand markets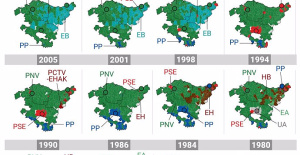 Historical results of the 2024 Basque elections, municipality by municipality
Historical results of the 2024 Basque elections, municipality by municipality Iran assures that any action by Israel will have an "immediate and highest level" response: "They will regret it"
Iran assures that any action by Israel will have an "immediate and highest level" response: "They will regret it" The Ciudad Real Court sentences the man who killed a thief with two shots in his home to 6 years
The Ciudad Real Court sentences the man who killed a thief with two shots in his home to 6 years PP and PSOE clash in the Senate over Koldo's appearance after a socialist writing on a work plan
PP and PSOE clash in the Senate over Koldo's appearance after a socialist writing on a work plan How Blockchain in being used to shape the future
How Blockchain in being used to shape the future Not just BTC and ETH: Here Are Some More Interesting Coins Worth Focusing on
Not just BTC and ETH: Here Are Some More Interesting Coins Worth Focusing on Valencia displays its "innovative and technological potential" at the Emerge Americas event in Miami
Valencia displays its "innovative and technological potential" at the Emerge Americas event in Miami The CSIC incorporates the challenges of robotics, nanotechnology and AI in the new strategic plan for biomedicine
The CSIC incorporates the challenges of robotics, nanotechnology and AI in the new strategic plan for biomedicine Innovation allocates 9.1 million to train 74,000 people and guarantee digital inclusion
Innovation allocates 9.1 million to train 74,000 people and guarantee digital inclusion LIFE SPOT manages to develop new green treatments that eliminate groundwater contamination
LIFE SPOT manages to develop new green treatments that eliminate groundwater contamination A million people demonstrate in France against Macron's pension reform
A million people demonstrate in France against Macron's pension reform Russia launches several missiles against "critical infrastructure" in the city of Zaporizhia
Russia launches several missiles against "critical infrastructure" in the city of Zaporizhia A "procession" remembers the dead of the Calabria shipwreck as bodies continue to wash up on the shore
A "procession" remembers the dead of the Calabria shipwreck as bodies continue to wash up on the shore Prison sentences handed down for three prominent Hong Kong pro-democracy activists
Prison sentences handed down for three prominent Hong Kong pro-democracy activists ETH continues to leave trading platforms, Ethereum balance on exchanges lowest in 3 years
ETH continues to leave trading platforms, Ethereum balance on exchanges lowest in 3 years Investors invest $450 million in Consensys, Ethereum incubator now valued at $7 billion
Investors invest $450 million in Consensys, Ethereum incubator now valued at $7 billion Alchemy Integrates Ethereum L2 Product Starknet to Enhance Web3 Scalability at a Price 100x Lower Than L1 Fees
Alchemy Integrates Ethereum L2 Product Starknet to Enhance Web3 Scalability at a Price 100x Lower Than L1 Fees Mining Report: Bitcoin's Electricity Consumption Declines by 25% in Q1 2022
Mining Report: Bitcoin's Electricity Consumption Declines by 25% in Q1 2022 Oil-to-Bitcoin Mining Firm Crusoe Energy Systems Raised $505 Million
Oil-to-Bitcoin Mining Firm Crusoe Energy Systems Raised $505 Million Microbt reveals the latest Bitcoin mining rigs -- Machines produce up to 126 TH/s with custom 5nm chip design
Microbt reveals the latest Bitcoin mining rigs -- Machines produce up to 126 TH/s with custom 5nm chip design Bitcoin's Mining Difficulty Hits a Lifetime High, With More Than 90% of BTC Supply Issued
Bitcoin's Mining Difficulty Hits a Lifetime High, With More Than 90% of BTC Supply Issued The Biggest Movers are Near, EOS, and RUNE during Friday's Selloff
The Biggest Movers are Near, EOS, and RUNE during Friday's Selloff Global Markets Spooked by a Hawkish Fed and Covid, Stocks and Crypto Gain After Musk Buys Twitter
Global Markets Spooked by a Hawkish Fed and Covid, Stocks and Crypto Gain After Musk Buys Twitter Bitso to offset carbon emissions from the Trading Platform's ERC20, ETH, and BTC Transactions
Bitso to offset carbon emissions from the Trading Platform's ERC20, ETH, and BTC Transactions Draftkings Announces 2022 College Hoops NFT Selection for March Madness
Draftkings Announces 2022 College Hoops NFT Selection for March Madness


























